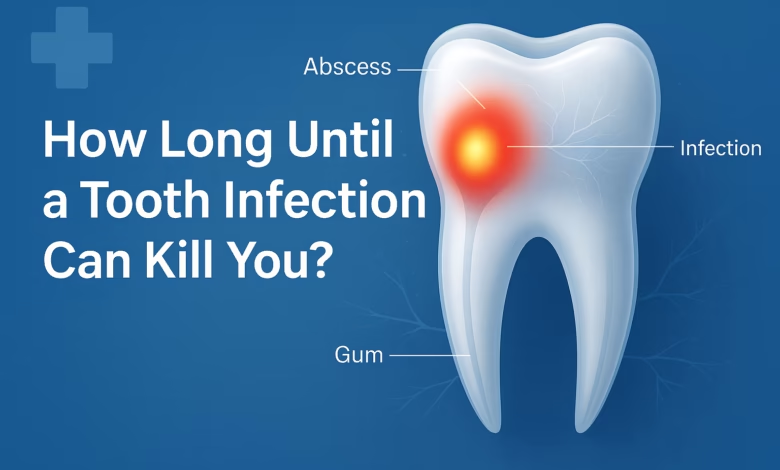
How Long Until a Tooth Infection Can Kill You?
Tooth Infection Risks: Timeline, Warning Signs & When to Act
Last Updated on November 29, 2025 by Prabhakar A
Wondering how long until a tooth infection kills you? The truth is, there’s no single answer, and that uncertainty is precisely what makes dental infections so nerve-wracking. Death from a tooth infection is rare (thankfully), but when it happens, it’s usually because someone either couldn’t access dental care or didn’t realize just how serious things had gotten.
In this guide, you’ll learn about the progression timeline of tooth infections, recognize critical warning signs that signal danger, understand which factors increase your risk of life-threatening complications, and discover exactly when you need to seek emergency care to protect yourself from severe outcomes like sepsis, airway obstruction, or brain infection.
The honest answer? There’s no fixed countdown clock. Some people live with an infected tooth for months before severe complications develop, while others, especially those with compromised immune systems, can deteriorate within days once the infection spreads beyond the tooth. In extreme cases, once bacteria enter critical areas like your bloodstream or airway, things can spiral frighteningly fast: we’re talking 48 hours in some documented instances.
Table of Contents
What is a Tooth Infection, from Decay to Abscess?
A tooth infection doesn’t just appear out of nowhere. It’s usually the ugly finale of a progression that started with something seemingly innocent: a cavity you meant to get filled but kept putting off, or maybe trauma from biting down on something hard.
Tooth decay marches through your tooth in stages. First, it attacks the enamel, that hard, protective outer shell. Then it burrows into the dentin, the softer layer underneath, which is when you start feeling sensitivity to hot or cold drinks.
When decay finally reaches the pulp (where all your nerves and blood vessels live), that’s when the real pain kicks in. At this point, bacteria have essentially set up camp inside your tooth, multiplying like crazy and forming an abscess, which is a pocket of pus that’s under pressure and looking for somewhere to go.
Dental trauma can fast-track this whole process. A cracked tooth from an accident or sports injury creates an express lane for bacteria to invade the pulp, potentially cutting what would’ve been months of gradual decay down to weeks or even days.
Do you know: 7 Home Remedies for Dealing with Toothache
How Dental Abscess Can Turn Into a Life-Threatening Condition?
An abscess isn’t just painful; it’s dangerous because it’s essentially a bacterial bomb waiting to spread. That pus building up? It’s full of bacteria, and when the pressure gets high enough or your immune system can’t contain it anymore, those bacteria start traveling.
And where they travel is what keeps dentists up at night. The infection can spread to your jaw, into the soft tissues of your neck (a condition called Ludwig’s angina, which sounds almost poetic until you realize it can block your airway), or even into your bloodstream.
Once bacteria hit your bloodstream, you’re looking at sepsis, which is a whole-body inflammatory response that can cause organ failure. Other nightmare scenarios include brain abscesses, endocarditis (infection of your heart valves), mediastinitis (infection in your chest), osteomyelitis (bone infection), and necrotizing fasciitis.
Here’s some perspective, though: modern antibiotics and surgical drainage have dramatically reduced death rates from dental infections. Ludwig’s angina, for instance, had a mortality rate above 50% before antibiotics became widespread; now it’s dropped to around 8-10% with proper treatment. But, and this is crucial, those statistics only apply when people actually get treatment.
Understanding How Long Until a Tooth Infection Kills You: Timeline Factors
So how long do you have? I wish I could give you a simple answer.
From the first twinge of tooth pain to abscess formation typically takes weeks to months if we’re talking about decay-related infections. In the first 24 to 48 hours, you might notice mild sensitivity or a dull, throbbing ache as the local infection begins inside the tooth. By days three to seven, abscess formation occurs as pus builds up, bringing increased swelling, bad taste, and more intense pain.
After one to two weeks, if left untreated, the infection can spread beyond the tooth into your face, jaw, or neck, causing facial swelling, difficulty opening your mouth, fever, and enlarged lymph nodes. The infection progresses through recognizable stages: in the first 1 to 3 days, you might notice soft, mildly tender swelling; by days 2 to 5, that swelling becomes hard, red, and severely painful; around day 5 to 7, you’ve got full abscess formation.
Here’s where it gets scary.
Once infection spreads to critical areas like your bloodstream, airway, or brain, deterioration can happen within days. Some medical sources document cases where people went from “this is getting worse” to life-threatening complications in as little as 48 hours. This unpredictable timeline is why understanding how long until a tooth infection kills you requires looking at individual risk factors rather than relying on a universal timeframe.
Why such variation?
Because everyone’s different. Your immune system strength, whether you have diabetes or other chronic conditions, the specific location of the infected tooth, which bacteria are involved, your age, all these factors influence how fast things progress. A healthy 25-year-old might fight off an infection for months before serious complications develop, while a 65-year-old with diabetes and heart disease might deteriorate in a week.
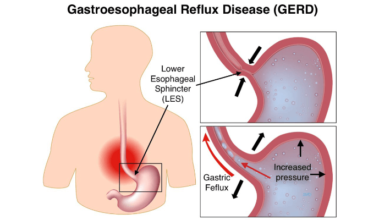
Know more: What Is GERD? How to treat the problem and overcome the symptoms?
Warning Signs & Danger Signals: When to Seek Emergency Care
Early symptoms of a tooth infection are pretty straightforward: throbbing pain that won’t quit, sensitivity to hot and cold, visible swelling around the tooth or gum, bad breath that doesn’t improve with brushing, maybe a bad taste in your mouth, swollen lymph nodes under your jaw.
But you need to know when things are escalating. Warning signs the infection is spreading beyond the tooth include fever, unusual fatigue, facial or neck swelling, difficulty swallowing, trouble opening your mouth all the way, persistent bad taste despite oral hygiene, and even tooth discoloration or looseness. These symptoms mean bacteria are moving into surrounding tissues.
Red-Flag Emergency Symptoms
Red-flag emergencies, and I mean drop everything and get to a hospital, include:
- High fever with chills
- Rapid heartbeat
- Difficulty breathing or swallowing (this could mean airway compromise)
- Severe swelling that’s spreading down your neck
- Confusion, dizziness, or altered mental state
- Extreme weakness
These are signs of sepsis or potential brain involvement. Don’t wait. Don’t assume it’ll get better on its own. Sometimes tooth pain actually decreases temporarily as the nerve dies, but the infection keeps spreading, so less pain doesn’t mean you’re out of danger.
Who Is at Higher Risk of Severe Complications?
Not everyone faces the same level of risk. People with weakened immune systems are particularly vulnerable: if you’re immunocompromised from medications, chronic illness, HIV, cancer treatment, or just older age, your body simply can’t fight infections as effectively.
Diabetes is a major risk factor because it impairs immune response and wound healing, plus high blood sugar creates an environment where bacteria thrive. Malnutrition, chronic alcohol use, and smoking all compromise your body’s ability to fight infection too.
Socioeconomic Barriers to Dental Care
Then there are access barriers that nobody really talks about enough. Financial constraints, lack of dental insurance, living in rural areas with dentist shortages, language barriers, cultural factors; all of these contribute to delayed care.
In the United States alone, approximately 57 million people live in dental health professional shortage areas, with 67% of those in rural communities. When you can’t afford a dentist or there isn’t one within 50 miles, a minor cavity becomes a ticking time bomb. Socioeconomically disadvantaged populations experience higher rates of untreated cavities and periodontal disease precisely because they face greater barriers to preventive and emergency dental care.
Treatment & Prevention: What to Do to Avoid Life-Threatening Consequences?
Good news: dental infections are highly treatable when caught early. Standard treatments include draining the abscess to relieve pressure and remove infected material, root canal therapy to save the tooth if possible, tooth extraction if the damage is too severe, and antibiotics to help your body fight the bacterial load.
Timing matters enormously. The earlier you seek treatment, the simpler and less invasive it is. A cavity caught early just needs a filling. An abscess caught before it spreads might only need drainage and antibiotics. But wait until the infection reaches your bloodstream or airway, and you’re looking at hospitalization, IV antibiotics, possibly surgery, and genuine risk to your life.
Prevention Strategies
Prevention is honestly pretty straightforward (even if following through isn’t always easy): brush twice daily with fluoride toothpaste, floss regularly, limit sugary foods and drinks, see your dentist for checkups even when nothing hurts, and address dental trauma immediately.
Emergency Interim Measures
If you’re in a situation where you can’t see a dentist right away, maybe it’s a weekend, maybe there’s a cost barrier, maybe you’re in a remote area, there are temporary measures: rinse with warm salt water to reduce bacteria, take over-the-counter pain relievers, avoid chewing on the affected side, stay hydrated. But please understand: these are temporary stopgaps, not solutions. You still need professional dental care as soon as humanly possible.
Do you know: 9 Healthy Foods That Are High in Vitamin C
Why There’s No Guaranteed “Death Date”: Understanding the Variability?
If you’re searching for a definite timeline, you’re not going to find one, because one doesn’t exist. Too many variables are in play: your baseline health, your immune system’s effectiveness, the specific bacteria involved, where in your mouth the infection started, whether you have underlying conditions like diabetes or heart disease, and how quickly you seek treatment all influence the trajectory.
Medical literature documents a wide range of outcomes. Some people live with low-grade dental infections for months before developing serious complications. Others progress from toothache to sepsis in under two weeks.
The documented cases of Ludwig’s angina (a particularly dangerous type of dental infection that spreads into the neck) show mortality rates varying from less than 1% in generally healthy populations with prompt treatment to over 23% in patients with significant comorbidities.
Myth vs. Reality: Common Misconceptions About Tooth Infections
Myth: “A tooth infection will kill you within a week.”
Reality: Death from dental infection is genuinely rare and typically requires prolonged neglect combined with vulnerable health status or barriers to care.
Myth: “Only elderly people need to worry about this.”
Reality: While older adults and those with chronic conditions face higher risk, anyone, including young, otherwise healthy individuals, can develop life-threatening complications from an untreated tooth infection.
Myth: “If the pain goes away, the infection is gone.”
Reality: This is perhaps the most dangerous misconception. Sometimes the nerve inside the tooth dies, which actually reduces pain temporarily. But the infection? It’s still there, still spreading, still dangerous. Decreased pain is not a reason to skip the dentist; it might actually be a sign things are getting worse.
When to Seek Medical/Dental Attention Immediately?
Don’t gamble with this. Seek immediate professional care if you experience:
- Persistent, severe tooth pain
- Visible swelling in your face, jaw, or neck
- Fever above 101°F (38.3°C)
- Difficulty swallowing or breathing
- Foul taste or smell that won’t go away
- Swollen lymph nodes
- Pain when opening your mouth
- Rapid heartbeat, confusion, or extreme weakness
Go to your dentist for dental-specific issues, but if it’s after hours or symptoms suggest systemic infection (fever, difficulty breathing, altered mental state), head to an emergency room. Early detection and treatment reduce the risk of severe complications by orders of magnitude. Hours can matter.
Also know: 7 Types of Cosmetic Dentistry Procedures
FAQ: Common Questions People Ask
Can a tooth infection kill you?
Yes, but it’s rare with modern medical care. Fatal outcomes typically occur when infections spread untreated to critical areas like the bloodstream, airway, or brain.
How long does it take for a tooth infection to become life-threatening?
There’s no single answer; it varies from days to months depending on your health, immune system, and whether you receive treatment. Once systemic spread occurs, deterioration can happen within 48 hours to a week.
What are the early signs I should not ignore?
Throbbing tooth pain, swelling, sensitivity, fever, bad breath or taste, and swollen lymph nodes under your jaw all warrant dental attention.
Can good oral hygiene alone prevent complications?
Good hygiene dramatically reduces your risk, but once an infection is established, you need professional treatment; brushing and flossing won’t cure an abscess.
What should I do if I can’t see a dentist right away?
Use warm salt water rinses, take over-the-counter pain medication, avoid the affected tooth when chewing, and seek dental care as soon as possible. These are temporary measures only.
Are some teeth more dangerous if infected?
Infections in lower molars are particularly associated with Ludwig’s angina due to their proximity to the floor of the mouth and submandibular space. But any tooth infection can potentially spread and become serious.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical or dental advice, diagnosis, or treatment. If you suspect you have a tooth infection, contact a dentist or healthcare provider immediately.
Comments
0 comments